Treating Diabetes
Insulin
Insulin is a hormone made by beta cells in the pancreas. When we eat,
insulin is released into the bloodstream where it helps to move glucose
from the food we have eaten into cells to be used as energy.
In people with type 1 diabetes, the body produces little or no insulin
as the cells that produce insulin have been destroyed by an autoimmune
reaction in the body. Insulin replacement by daily injections is
required.
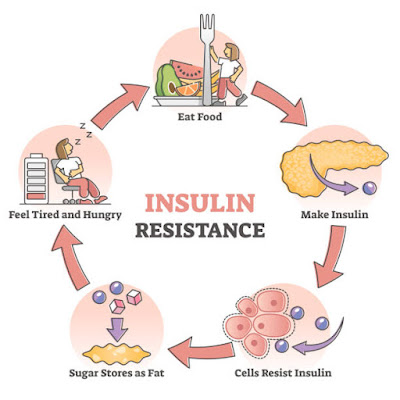
In people with type 2 diabetes, the body produces insulin but the
insulin does not work as well as it should. This is often referred to as
insulin resistance. To compensate the body makes more but eventually
cannot make enough to keep the balance right. Lifestyle changes can
delay the need for tablets and/or insulin to stabilize blood glucose
levels. When insulin is required, it is important to understand that
this is just the natural progression of the condition.
Insulin: The Holy Grail of Diabetes Treatment
RMIT University has produced a short overview of insulin, a drug that keeps in excess of one million Australians alive. Watch the video to understand why insulin is important and why so many Australians rely on it to stay alive. Copyright © 2015 RMIT University, Prepared by the School of Applied Sciences (Discipline of Chemistry).
Administering Insulin
At this stage, insulin can only be injected. Insulin cannot be given
in tablet form as it would be destroyed in the stomach, meaning it would
not be available to convert glucose into energy.
Insulin is injected through the skin into the fatty tissue known as the
subcutaneous layer. You do not inject it into a muscle or directly into
the blood. Absorption of insulin varies depending on the part of the
body into which you inject. The tummy (abdomen) absorbs insulin the
fastest and is the site used by most people. The buttocks and thighs are
also used by some people.
While it is essential to give each injection in a slightly different
spot within one site, it is not advisable to change sites without first
discussing it with your doctor or Credentialled Diabetes Educator.
The range of injection devices and tiny needles available today make
injecting insulin much easier than most people imagine. When starting
insulin, your doctor and Credentialled Diabetes Educator will help you
adjust to the new routine and task of giving insulin and find the right
dose to reduce your blood glucose levels to acceptable levels.
Insulin Syringes
Insulin can be injected by an insulin syringe, an insulin pen with a
fine needle, or via an insulin pump. Each method is chosen for a
particular purpose and based on an individual’s needs.
Insulin syringes and insulin pens (pen needles) are currently the most
common way of administering insulin. Injection devices are made in
different sizes, and the size used depends on the quantity of insulin
being injected. To avoid under or over-dosing, it is important that you
know how to measure the insulin dose in your device. Your Credentialled
Diabetes Educator can help you with this. Syringes should only be used
once, and then disposed of in an appropriate syringe disposal unit.
Insulin Delivery Devices (pens)
Many people find pen devices easier and more convenient to use than
syringes. If you have difficulties with your sight or have problems with
arthritis you may find a pen device easier to use. Pen devices are
available in different shapes and sizes. An insulin cartridge (3 ml,
containing 300 units of insulin) fits into the device. When finished, a
new cartridge is inserted. Some pen devices, however, are pre-filled
with insulin and the whole device is disposable. Your doctor or
Credentialled Diabetes Educator will advise the one that’s right for
your needs and lifestyle.
Syringes and pen needles are free for people registered with the National Diabetes Services Scheme (NDSS).
Types of Insulin
When you take insulin it acts to reduce the level of glucose in your
blood. When glucose is at its lowest level, the effect of the insulin is
said to have reached its ‘peak’. After this, the effect gradually wears
off and blood glucose levels rise.
Your doctor or Credentialled Diabetes Educator will work out with you what type of insulin is right for you.
- Fast-acting insulin is clear in appearance and starts to work from 1 to 20 minutes. It peaks approximately 1 hour later and lasts from 3 to 5 hours. You must eat immediately after injecting fast-acting insulin.
- Short-acting insulin is clear in appearance. It begins to work within half an hour, so you need to inject half an hour before eating, and it peaks at 2 to 4 hours and lasts for 6 to 8 hours.
- Intermediate-acting insulin is cloudy in appearance and has either protamine or zinc added to delay its action. It begins to work about 1 and a half hours after injecting, peaks at 4 to 12 hours, and lasts for 16 to 24 hours. Before injecting, check the leaflet included in the pack for instructions on preparing the insulin.
- Mixed insulin is cloudy in appearance and contains pre-mixed combinations of either fast-acting or short-acting insulin and intermediate-acting insulin. This makes injecting easier by giving two types of insulin in one injection. This insulin can be taken before a meal to provide a stable level of insulin for some time after the meal. Before injecting, check the leaflet included in the pack for instructions on preparing the insulin.
- Long-acting insulin is clear in appearance. It typically has no pronounced peak and lasts for up to 24 hours.








Comments
Post a Comment